Free Wv Peia Prior Authorization Form
Navigating the healthcare paperwork can often be a complicated and daunting task for both healthcare providers and patients. One such critical document within the West Virginia Public Employees Insurance Agency (PEIA) system is the Prior Authorization form. This essential form serves as a gatekeeper, determining whether certain medications or medical services will be covered under the patient's insurance plan based on medical necessity and policy compliance. Located in Morgantown, WV, and facilitated by the WVU School of Pharmacy, the processing of this form involves the thorough verification of the requested service or medication, requiring detailed information from the prescribing healthcare provider. The form mandates the inclusion of specific details such as the dispensing pharmacy's National Association of Boards of Pharmacy (NABP) Number, pharmacy name, and address, along with the patient's personal and medical details. Healthcare providers must send the completed form via fax or mail, emphasizing the importance of accuracy and completeness to avoid delays in treatment due to administrative hurdles. As patients await these approvals, understanding the Prior Authorization form's significance and requirements becomes crucial in ensuring timely access to necessary healthcare services.
Wv Peia Prior Authorization Example
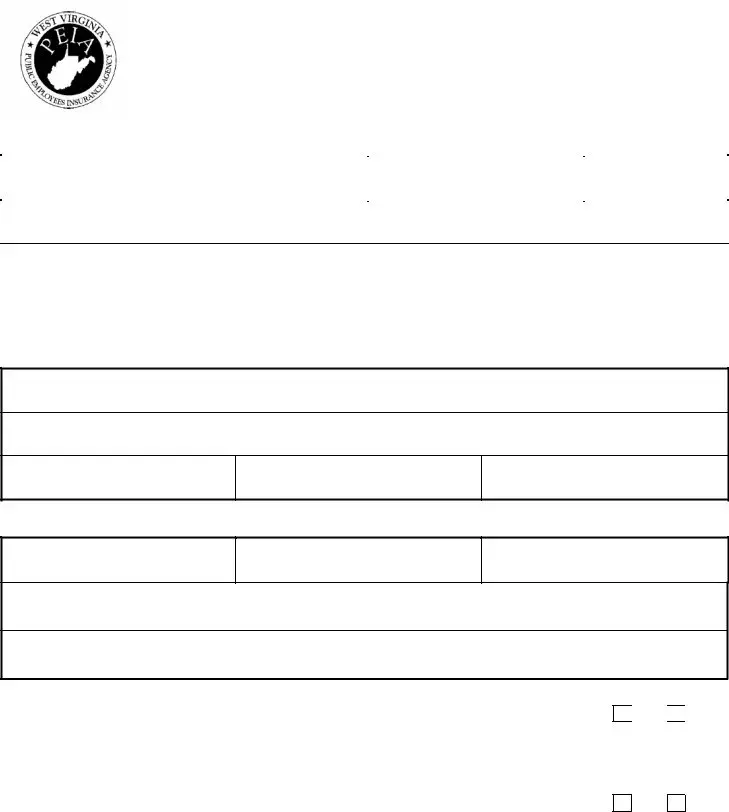
!
PO Box 9511 HSCN, WVU School of Pharmacy
Morgantown, WV 26505
PHONE |
FAX: |
|
!7$ |
|
|
&$$##$"$ |
|
|
$$8$98$989 |
$$:#$"$;% |
$$:$"<$ |
|
|
|
|
|
|
7$##$% |
$ |
|
|
||
|
|
|
""$ #% |
8$9#8/6/9 |
|
|
||
|
||
|
||
|
|
|
|
|
|
&"$
$$
$ ;
$>;
& "$8"(?9
Dispensing Pharmacy NABP Number
Pharmacy Name:
$ ;
$>;
Pharmacy Address (Street) |
(City) |
(State) |
(Zip) |
&? "$ "?7$"7$&
.&+$ $$$$#"$ #?$ $ #$89@
")'$$ $$ $$ "##$ #$? $ "#$ &
) |
|||
A&$ $ $$ $!$$ "$ #$89$ $#$7@
)
8"$$#'$ $ $$$$$ $'$$"$ $$$$9
"#$$$% #$$ $$"#$"$$$ #&
"$$##"$ "$ #!#$$#!&"$$ $##$'
$"#$ $#'#$$$$($ $$"$ #$$$ $#&" !
!#$ $'$"$ ##$$"$"$ #$&
Form Specifications
| Fact Number | Detail |
|---|---|
| 1 | The form is used for Prior Authorization requests. |
| 2 | It is managed by the WVU School of Pharmacy located in Morgantown, WV. |
| 3 | For inquiries, a phone number is provided: 1-800-847-3859. |
| 4 | Documents can be sent via fax to 1-800-531-7787. |
| 5 | It is specific to West Virginia, as indicated by its address and governing state-specific laws. |
| 6 | Information required includes the dispensing pharmacy NABP number and pharmacy name. |
| 7 | Pharmacy address must include street, city, state, and ZIP code. |
| 8 | The form includes sections for medication information and patient details. |
| 9 | Governing laws for the form include state-specific regulations for medical authorizations in West Virginia. |
Guide to Filling Out Wv Peia Prior Authorization
Once you've determined the need for completing the WV PEIA Prior Authorization form, understanding the process is your next step. This guide will help fill out the form accurately. Please gather all necessary patient information and medication details before you begin. The authorization process involves providing specific information to ensure the patient receives coverage for the prescribed medication or service. Follow these instructions to complete the form.
- Start by writing the recipient address: PO Box 9511 HSCN, WVU School of Pharmacy Morgantown, WV 26505 at the top of your cover letter or envelope.
- Include the contact information: Phone: 1-800-847-3859, Fax: 1-800-531-7787 on your correspondence.
- Input the dispensing Pharmacy NABP Number in the designated space.
- Fill in the Pharmacy Name, Address (Street, City, State, Zip) in the corresponding sections.
- Provide detailed information regarding the patient and the prescriber, including IDs, names, and contact details in the sections prompted.
- Specify the medication requested, along with strength, dosage form, and quantity.
- Include any additional relevant clinical information or justification for the medication requested to support the prior authorization request.
- Ensure that the prescriber signs and dates the form to validate the request.
- Review the form for accuracy and completeness. Incomplete or inaccurate forms may result in delays.
- Send the completed form via fax to 1-800-531-7787, or if instructed, mail it to the provided PO Box address.
After submitting the form, it's important to wait for communication from WV PEIA regarding the authorization status. This process can take several days. During this time, keep a copy of all submitted documents for your records. Pay close attention to any additional requests or instructions from WV PEIA to ensure a smooth process for obtaining the necessary authorization for the patient's medication or service.
Things You Should Know About Wv Peia Prior Authorization
What is the WV PEIA Prior Authorization form?
The WV PEIA Prior Authorization form is a document required by the Public Employees Insurance Agency (PEIA) in West Virginia to gain pre-approval for certain prescriptions or medical services before they are provided. It ensures that the prescribed treatment or medication is covered under the insurance plan and is medically necessary.
How do I submit a WV PEIA Prior Authorization form?
Submission can be done by filling out the form with all the required information and sending it to the specified address: PO Box 9511 HSCN, WVU School of Pharmacy, Morgantown, WV 26505. Alternatively, it can be faxed to 1-800-531-7787. The form requires information from both the prescribing healthcare provider and the dispensing pharmacy.
Who needs to fill out this form?
Both the healthcare provider prescribing the medication or service and the pharmacy dispensing it must complete their respective sections of the form. The healthcare provider will need to provide detailed information about the medical necessity, while the pharmacy must supply its contact and licensing information.
What information is required from the dispensing pharmacy?
The pharmacy is required to fill in details such as the National Association of Boards of Pharmacy (NABP) Number, the pharmacy's name, address, and contact information. This ensures the pharmacy is recognized and approved to dispense medication under PEIA coverage.
Can I submit the form without a dispensing pharmacy NABP Number?
No, the dispensing pharmacy's NABP Number is crucial for processing the form. It identifies the pharmacy within the national database, verifying its authorization to dispense medications. Without this number, the submission may be considered incomplete and could be denied.
What happens if I don't get prior authorization?
Without prior authorization, the prescribed medication or service may not be covered under the PEIA plan. This can lead to out-of-pocket expenses for the patient. In some cases, the service or medication might be completely unavailable without the necessary approval.
How long does it take to get a response for a prior authorization request?
Response times can vary depending on the complexity of the request and the volume of submissions. However, the PEIA strives to process requests promptly. Contacting the PEIA directly at 1-800-847-3859 may provide a more specific timeframe for your individual request.
Is there a way to expedite the prior authorization process?
In cases where immediate treatment is necessary, healthcare providers may reach out to the PEIA to discuss the urgency of the situation. While expedited processes exist, they are typically reserved for emergency situations and require detailed justification for the urgency.
What should I do if my prior authorization request is denied?
If your request is denied, the PEIA provides guidance on how to appeal the decision. It involves submitting a formal appeal that includes any additional information or clarification that might support the necessity of the medication or service. Instructions for appeals are available from the PEIA.
Common mistakes
Completing the WV PEIA Prior Authorization form requires careful attention to detail. Unfortunately, several common mistakes can lead to delays in the authorization process, potentially impacting timely access to necessary medications or services. Below is a list of some common errors to avoid.
- Not providing complete contact information: The form requires details such as the pharmacy's phone and fax numbers. Leaving these fields blank or entering incomplete information can prevent timely communication.
- Incorrect Dispensing Pharmacy NABP Number: This is a unique identifier for pharmacies. Entering this number inaccurately can lead to confusion and delays in processing the authorization.
- Failing to specify the medication or service required: Clearly indicating the name and dosage of the medication, or detailing the specific service needed, is crucial. Ambiguities here can result in back-and-forth communication for clarification, delaying approval.
- Omitting the patient’s information: Complete patient details, including their full name and date of birth, are essential. This information must match what is on file with PEIA to ensure the authorization is processed for the correct individual.
- Forgetting to include the prescribing physician's details: The form requires information about the physician who is prescribing the medication or recommending the service. This includes their name, contact information, and sometimes their NPI (National Provider Identifier) number.
- Submitting outdated or incomplete forms: Always ensure you are using the most current version of the prior authorization form and that all sections relevant to your request are completed in full.
To avoid these common mistakes, it’s important to:
- Review the entire form before submission to ensure that no required fields are missed.
- Double-check all entered information for accuracy, especially identifiers like the NABP Number.
- Ensure that the form used is the latest version, which can usually be found on the WV PEIA’s website or by contacting them directly.
- Keep a copy of the completed form for your records and future reference.
By being diligent and mindful of these guidelines, you can help streamline the prior authorization process, facilitating quicker access to necessary medications or services for patients under WV PEIA coverage.
Documents used along the form
When handling the complexities of medical processes, particularly with the West Virginia Public Employees Insurance Agency (WV PEIA), certain forms and documents are crucial for smooth operations. The WV PEIA Prior Authorization form is just the beginning. Alongside this vital document, several others play key roles in ensuring that patients receive the care they need without unnecessary delays. Below is a list of other forms and documents often used in conjunction with the WV PEIA Prior Authorization form, each serving its unique purpose in the healthcare continuum.
- Medical Necessity Letter: This document is written by the healthcare provider to explain why a specific treatment, test, or procedure is essential for the patient's health. It supports the prior authorization request by providing clinical justifications.
- Appeal Form: If a prior authorization request is denied, patients or providers can use this form to contest the decision. It requires detailed information on why the treatment should be considered necessary.
- Prescription Drug Claim Form: For medications that may not initially qualify for coverage, this form is used for reimbursement requests. It is filled out after the medication has been purchased.
- Member Reimbursement Form: Patients use this form to request reimbursement for medical expenses they've paid out-of-pocket. It often requires receipts or other proof of payment.
- Provider Information Form: This details the healthcare provider's information, including credentials, contact details, and specialization. It is important for verifying the provider's eligibility to request certain treatments or medications.
- Treatment Plan Form: A comprehensive outline of the proposed treatment strategy, including medications, procedures, and any other relevant healthcare interventions. This form helps the insurance assess the necessity and efficiency of the suggested plan.
Together, these documents create a more complete picture of the patient's healthcare needs and circumstances. They ensure that every angle is considered in the prior authorization process, thus facilitating better communication between healthcare providers, patients, and insurance entities. Understanding the purpose and proper usage of each form can significantly enhance the efficiency and outcome of healthcare services for those covered by WV PEIA.
Similar forms
The Medicare Prior Authorization Request Form bears strong similarities to the WV PEIA Prior Authorization Form in terms of both function and structure. Designed specifically for Medicare-covered services, this document plays a crucial role in ensuring that certain medications or treatments receive prior approval before they are dispensed to the patient, similar to how the WV PEIA form functions for patients under the Public Employees Insurance Agency in West Virginia. The emphasis on prior approval helps manage healthcare costs and ensure the appropriateness of prescribed treatments, echoing the objectives of the WV PEIA form.
The Prescription Drug Prior Authorization Request Form, commonly used in private healthcare insurance, resembles the WV PEIA Prior Authorization Form in its aim to manage healthcare costs efficiently. By requiring a healthcare provider to justify the need for a specific medication before it is dispensed, this document helps prevent unnecessary expenditure on expensive or unneeded drugs. This process parallels the WV PEIA's approach, facilitating a careful review of medications or treatments to ensure they align with the patient's health needs and insurance policy provisions.
The Medicaid Prior Authorization Form is another document with notable similarities to the WV PEIA Prior Authorization Form. Employed within the Medicaid program, it seeks to ensure that recommended treatments or medications are medically necessary and cost-effective before approval. This measure is pivotal in controlling the program's expenditure, whereby it mirrors the cost-containment and medical necessity verification functions of the WV PEIA form, underscoring both forms' roles in promoting responsible healthcare spending and utilization.
Finally, the Health Service Request Form used by many healthcare management organizations (HMOs) shares a common goal with the WV PEIA Prior Authorization Form. This document streamlines the process of requesting and approving medical treatments, surgeries, or diagnostic tests. By integrating such a systematic approach, it not only aids in managing resources but also ensures that patients receive medically necessary services. This parallels the WV PEIA form's objective of securing prior approval to optimize patient care while addressing the imperative of cost management within the healthcare system.
Dos and Don'ts
When it comes to completing the WV PEIA Prior Authorization form, ensuring accuracy and attention to detail is crucial. The process can be streamlined by adhering to a list of do's and don'ts. Here are some guidelines to help you navigate the completion of this form:
Do:
- Double-check the accuracy of all entered information, including the PO Box, phone, and fax numbers provided on the form. Mistakes in these details can lead to processing delays.
- Ensure that the dispensing pharmacy’s NABP Number, along with the pharmacy name and address, is correctly filled out. This information is vital for the authorization process.
- Include all necessary documentation that supports the prior authorization request. This could include clinical notes or lab results that justify the need for the prescribed medication or treatment.
- Retain a copy of the completed form, and all supporting documents, for your records. This will be helpful if there is a need to follow up or if any issues arise during the processing of the authorization.
Don't:
- Leave any section blank. Incomplete forms may result in rejection or significant delays in processing. If a section does not apply, it's better to mark it as "N/A" than to leave it empty.
- Forget to sign and date the form. An unsigned form is often considered incomplete and will not be processed until it is properly signed.
- Use outdated forms. Always verify that you are using the most recent version of the form, as using an outdated form can lead to delays or denial of the authorization.
- Assume the submission has been successful without confirmation. Always follow up with the WV PEIA to ensure the form has been received and is being processed.
Misconceptions
When it comes to handling the West Virginia Public Employees Insurance Agency (WV PEIA) Prior Authorization form, there are several misconceptions that need clarification. Understanding these can save time and ensure smoother processing for healthcare providers and their patients.
- Misconception 1: Any medication needs prior authorization.
Not all medications require prior authorization. The WV PEIA has a specific list of drugs that require this step. Medications not on this list can be prescribed and dispensed without the need to complete this form.
- Misconception 2: The process is too complicated and time-consuming.
While the prior authorization process involves several steps, the goal is to ensure that patients receive medications that are both effective and safe. By closely following the guidelines and providing complete information, healthcare providers can streamline the process.
- Misconception 3: Prior authorization is only about controlling costs.
Cost control is a factor, but the primary intent of prior authorization is to ensure patient safety and appropriate medication use. It's a measure to avoid unnecessary medication exposure and to ensure that prescribed medications are in line with evidence-based guidelines.
- Misconception 4: The decision is final and cannot be appealed.
If a prior authorization request is denied, healthcare providers have the right to appeal the decision. There's a structured appeal process in place, allowing for the review of the initial decision and the provision of additional information that may support the authorization request.
- Misconception 5: The form is only for pharmacists.
While the dispensing pharmacy's information is required, the completion and submission of the form are primarily the responsibilities of the prescribing healthcare provider. It is essential for ensuring that patients receive the correct medications in a timely manner.
Clearing up these misconceptions can lead to better communication between healthcare providers, pharmacists, and insurance agencies, ultimately benefiting patient care.
Key takeaways
Understanding how to correctly fill out and use the West Virginia Public Employees Insurance Agency (WV PEIA) Prior Authorization form is essential for ensuring timely access to covered medical services or prescriptions for patients. Here are key takeaways for healthcare providers:
- Prior to submission, ensure all required sections of the form are thoroughly completed to avoid delays. Any missing or inaccurate information can lead to the rejection of the authorization request.
- The form requires specific details, including the Dispensing Pharmacy's National Association of Boards of Pharmacy (NABP) Number, Pharmacy Name, and complete Pharmacy Address. Accurately providing these ensures the medication is correctly processed and dispensed.
- Contact information, including the fax number and phone number provided on the form (1-800-847-3859 for phone and 1-800-531-7787 for fax), is important for any follow-up or clarification needed by WV PEIA during the authorization process.
- The prescriber's details are mandatory; ensuring these are filled in correctly enables the PEIA team to contact the prescriber if additional information is needed or to notify them of the authorization’s status.
Adhering to these key points when handling the Prior Authorization form is vital for healthcare providers to facilitate their patients' smooth and efficient access to necessary treatments covered by WV PEIA.
Popular PDF Forms
Wv State Tax Forms - Adaptable for reporting final or amended production figures, catering to needs for correction or update.
What Happens If You Don't Return License Plates in Va - The WV-4S form is an essential document for any vehicle owner in West Virginia who needs to declare a registration plate missing or stolen.